Can Your Daily Choices Influence if You Develop an Autoimmune Disease?
In the spirit of rounding out a series of autoimmune disease posts, this post will highlight the role that environmental triggers play in the development and healing of Autoimmune disease.
Environmental triggers are perhaps the most compelling reason to continue to educate, empower and inspire regarding autoimmune disease development and healing. This is because they are largely based on our daily choices and, thus, modifiable.
They also greatly influence the development of enhanced intestinal permeability, another part of the triad, as our daily choices contribute to whether or not we develop a leaky gut. More importantly, how we heal it will also begin to heal autoimmune disease.
Where do environmental triggers fit into the puzzle that is Autoimmune Disease?
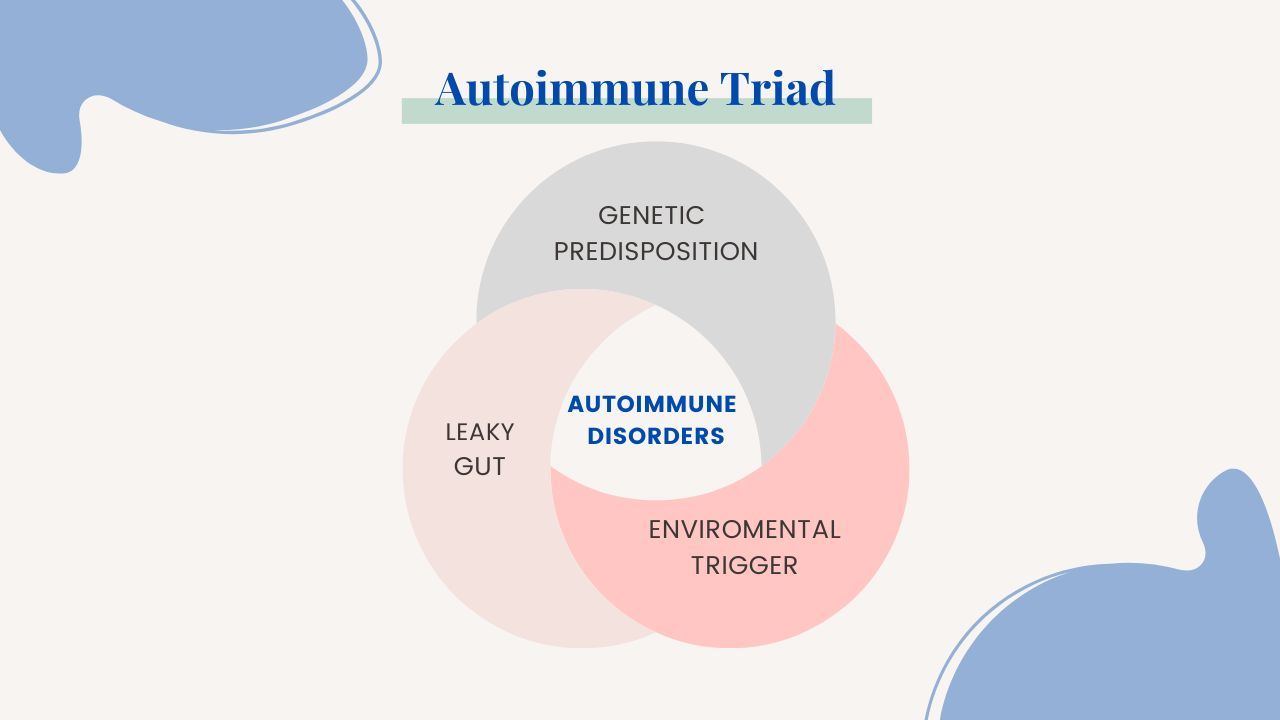
We know that autoimmune disease is inflammation stemming from a problem with our immune system. It occurs when our immune system has become hypervigilant and dysregulated. It may even be considered confused as it is targeting a response to our own tissue and organs. While genetic predisposition is a factor, something in the environment which leads to a leaky gut is present as well and more impactful, creating the autoimmune triad and a perfect storm leading to Autoimmune disease. This dysfunction sets the stage for the spectrum of inflammation and immune system response to our own tissue. It can be any tissue. Some common ones that we develop autoimmunity to are:
- Thyroid in Hashimoto’s thyroiditis or Grave’s disease
- Joints in Rheumatoid Arthritis or Psoriasis
- Protective covering of our nerve cells and brain in Multiple Sclerosis
- Intestines in Celiac disease, Ulcerative colitis and Crohn’s disease
- Skin in Psoriasis or vitiligo
- Multiple organs and tissues in Lupus
A genetic predisposition is not enough to produce disease. The gene must be activated or “turned on”. Several factors influence this, but lifestyle and daily choices are key. These triggers influence development of enhanced intestinal permeability or leaky gut. This happens when the gut lining is worn down and becomes leaky.
These triggers essentially poke holes in our gut lining. The gut microbiome also becomes imbalanced which can be a trigger in and of itself.
Why is the gut the hub?
Since more than 70% of our immune system sits in our gut, this amplifies its reaction and makes our systemic immune response hypervigilant to things with which the body would normally not have to contend. If the gut was in good shape the immune system would function as expected, which is to tolerate most of what it encounters. There are levels of protection that we rely upon to keep us safe. An optimally functioning immune system takes care of a threat, if need be, swiftly and effectively. But most things are now perceived as threats and most people’s immune system’s aren’t functioning optimally. They can include such things as:
- Pathogenic microbes such as bacteria such as H. pylori
- A “not so well chewed” piece of food can also pass through and provoke an immune response - this is why it’s so important to see your food, smell your food and really chew your food well.
- Dander or saliva from beloved pet
All of these daily, persistent exposures stress the gut and immune system. Think of them as chronic damage doers breaking down one of the key barriers to protect us.
Leaky gut happens when for a whole host of reasons some of which are:
- Diet high in processed and refined foods such as sugars and starches
- Medications such as antibiotics
- Vitamin D deficiency
- Stress - both mental/emotional such as the loss of a loved one or livelihood and physiological such as acute or chronic infection, allergies or sensitivities, or trauma
Avoiding or healing leaky gut is paramount. Here’s a start:
- Ditch the refined/processed foods and opt instead for a nutrient dense/whole foods diet. This is the biggest positive lifestyle choice
What are some triggers that are considered environmental in the development of autoimmune disease?
The third part of the triad is exposure to environmental triggers. It can be a single trigger or multiple ones which is more likely given our exposure in this modern day world. Here are some common food and toxins that trigger autoimmunity:
- Gluten or other commercial crops which also contain toxins such as glyphosate
- Mycotoxins found in commercial foods such as coffee, peanuts, dried fruit
- Heavy metals including mercury found in silver fillings or certain fish such as tuna
- Common household plastics including BPA
- Commercial household chemicals contained in everyday products such as formaldehyde found in glues, cleaning products, detergents and personal hygiene products including Trichloroethylene and Ethylene oxide
- Medications such as antibiotics
- Cigarette smoke
- Nail polish
There is emerging data to suggest that high salt intake may drive the progression and severity of autoimmune disease by impacting key interactions with immune molecules within the gut. It will be interesting to follow this data trend.
Why learning about triggers is important…
We must stay on our toes when it comes to environmental exposures that could trigger autoimmune disease. But there is a balance. It is important to avoid and mitigate as much exposure as possible but complete avoidance is impossible. This can be accomplished by being intentional with lifestyle choices and also being a savvy consumer who knows their way around ingredient lists and content labels. This will likely mean buying organic or locally sourced and trusted food when it is within means. This is the best way to ensure that you are getting the cleanest foods possible. It can mean ensuring that your conventional dentist isn’t placing amalgam fillings but rather non-mercury options, such as resin composite, if cavities are detected. It can also mean having a conversation with your doctor about why he/she may not prescribe an antibiotic for an illness that is likely to be viral. Hopefully, their professional opinion takes antibiotic stewardship into account. This doesn’t mean not prescribing an antibiotic when it is warranted, such as for a known or suspected bacterial infection; it just means using sound and reasonable judgment when it comes to prescribing antibiotics. Data suggests that most antibiotic prescriptions are not warranted and are likely contributing to dis-ease and imbalanced states as opposed to “curing” infection. Seeking conventional healthcare should be less about “giving the people what they want'' and more about educating them about the particular imbalance that they may be experiencing while providing appropriate care. In an age of 8 min appointments and no time or energy for discussion or education a prescription for an unnecessary medication is often what’s on offer.
But, you can do better. And you deserve better.
Continuing to be inspired and empowered through education will serve you - always. Learning to connect the dots will actually send signals of safety to your body; even as you continue to work through the dynamics.
Is chronic bloating a regular part of your life? Well it doesn't have to be.
Chronic bloating may be common, but it is NOT normal!
Bloating itself isn't the problem, it's usually a sign that something deeper is going on. Watch this free one hour masterclass and learn the 4 main types of bloating, their causes and what you can do to become bloat free for good!

